Saving Lives through Test and Treat: Lessons Learned from Option B+
At the 8th International AIDS Conference (IAS) Conference in Vancouver, the results of the START study have been released and provided a solid platform for the global HIV community around the to move HIV treatment paradigm to a Test and Treat approach. Under this approach, all HIV-positive individuals would be eligible for antiretroviral therapy (ART) at the time of diagnosis. The benefits of this approach would be to better and earlier protect the immune system, preventing long term morbidity and mortality and preventing spread of HIV within the communities. This new approach has the potential to dramatically slow the HIV epidemic — a critical step toward ending AIDS by 2030.
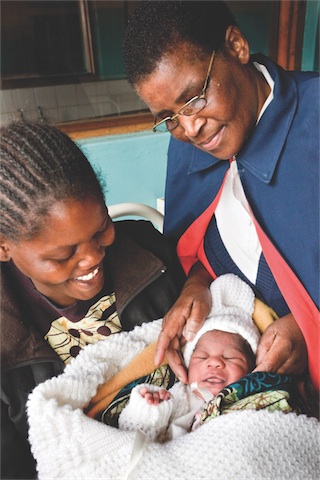
In recent years, EGPAF has led the way in implementation of Option B+, in which all HIV-positive pregnant and breastfeeding women are put on lifelong ART, which in a way already represents a Test and Treat approach. Option B+ helps keep mothers alive and protects their baby from HIV transmission. Keeping HIV-infected mothers healthy and on treatment is also critical to the survival of all their infants, whether HIV-positive or HIV-negative. Option B+ has been effective in reducing mother-to-child transmission (MTCT) rates in countries that have implemented it. In Malawi, where Option B+ was developed, the national MTCT rate at six weeks is reported to be 3.7%, a huge reduction from the MTCT rate seen before Option B+ rollout.
With Option B+, women are able to initiate ART on the same day as their diagnosis, since there are no longer any other criteria for treatment eligibility. Some newly diagnosed pregnant women need time to accept their HIV status and to disclose to their families; some have reported feeling overwhelmed when also asked to begin ART on the same day. Several countries have found that as many as 10-20% of HIV-positive pregnant women are not returning for a second antenatal care (ANC) visit after being initiated on ART. There is an urgent need to address these barriers to early retention for these newly diagnosed mothers. Some countries have also reported that women whose HIV disease is not advanced are stopping their treatment after the breastfeeding period ends and the perceived risk of transmitting the virus to the infant is gone.
Helping the women to remain on treatment for their own health is an important component of EGPAF’s mission. EGPAF programs have put interventions in place to provide better counseling and support to pregnant women, as well as making clinic services more efficient, improving documentation and reporting, all of which are improving access and retention on Option B+.
In addition to retaining the women on treatment, follow -up of HIV-exposed infants remains a challenging task. There are many reasons for this, including the lack of linked (mother/infant) medical records, separate service points for women and children, and lack of understanding of women on the importance of the follow-up for infant testing. When these infants become lost to follow up care, those who become HIV-positive miss the opportunity to access lifesaving treatment. For those HIV-positive infants and children who are identified, the proportion of those who are initiated on ART remains low. In Tanzania and Uganda, EGPAF capitalized on the Option B+ rollout to also identify and overcome barriers to retention of mother-baby pairs in care. These lessons have been shared across our EGPAF country programs.
As Option B+ was rolled out, it became apparent that community support of the new approach was critical to its success. Fear of stigma or abandonment led some newly identified women to discard their lifesaving drugs. In Malawi, some health care workers reported that they took it upon themselves to educate the community, which improved acceptance of the women taking ART and increased retention in care. In other countries, such as Lesotho and Uganda, large community campaigns were undertaken to sensitize communities about the upcoming changes. Acceptance of Option B+ was high in both these countries from the very beginning of the rollout and community knowledge was also noted to be high.
Important lessons have been learned through implementation of Option B+ that might become useful for the roll out of the Test and Treat approach, and include: intensified counseling and support are required at the time of HIV diagnosis, timely linkage to care and sustained retention require vigorous monitoring and support , and community knowledge, engagement an d support are crucial to support changing guidelines. As we move towards a Test and Treat approach where treatment will become available to all people living with HIV, the Option B+ lessons will be important to bring to the attention of the global community, ministries of health, and other stakeholders.
Mary Pat Kiefer, Senior Director of Technical Leadership Development, EGPAF
General


